The transformation in healthcare is no longer gradual and not silent, but real-time.
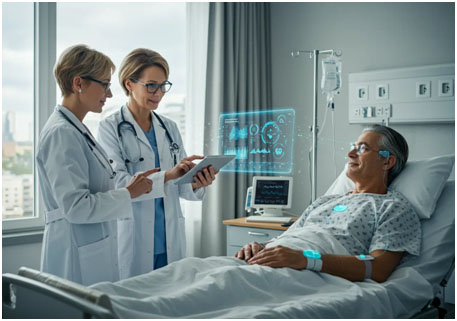
Generative AI is currently actively involved in the way individuals perceive their symptoms, manage conditions, and interact with medical systems across hospitals, clinics, telehealth platforms and personal devices. In the heart of this change is ChatGPT Health, a niche adaptation of the conversational AI that is part of a broader trend transforming modern medicine.
It is not a scenario that will happen in the distant future. It is happening now.
Physicians read AI summaries prior to patient visits. During the peak periods, nurses depend on the automated triage systems. Given that patients have the next appointment, they process the test results with the help of AI tools. Generative models are used in health systems to minimize paperwork rather than people.
AI in healthcare is no longer an experiment in 2026. It is operational.

Healthcare is changing in real time. Generative AI now supports doctors, nurses, and patients across hospitals, clinics, and digital care, with ChatGPT Health at the centre of this shift. (Image Source: Intelligent CIO)
What is ChatGPT Health, and Why Does it Matter Now
ChatGPT Health is a wider category of health-related generative AI bot systems aimed at assisting medical dialogue, clinical processes, and patient education with an increased level of care, context, and precision.
Unlike general chatbots, they focus on:
- Understanding of medical language.
- Evidence-based responses.
- Context awareness.
- Safety guardrails.
- Clear limitations.
This is not aimed at displacing clinicians. This is aimed at making better decisions, quicker work and clearer communication.
Overload in healthcare has been a thorn in the flesh of the healthcare environment since time immemorial; there are too many patients, too much data, too little time. Generative AI fills this point of pressure, not as a miracle solution, but as a useful tool.
And timing matters.
The healthcare systems in the world experience a lack of staff, increased expenses, declining age, and the increasing demands of personalised care. The adoption of AI is not happening fast because it is a trendy practice, but also because the system requires some offloading.
The Reason Why 2026 is a Turning Point for AI in Medicine
The AI healthcare discussion has changed. Previous arguments revolved around the question of whether AI would be beneficial. The modern discourse revolves around how it can and will be deployed in an irresponsible manner.
This moment is driven by three forces:
The Size Of Data Has Become Uncontrollable
The rate of medical data is increasing at a faster rate compared to the speed of the human team. Healthcare systems receive images, laboratory findings, genomics, clinical records, and wearable information every day. Generative AI is well placed in this environment, identifying patterns, summarising insights and pointing out risks within seconds.
Patients Demand More Access
Waiting in a queue to get simple information is no longer accepted by patients. They desire transparency, speed, and e-commerce. Artificial intelligence tools have now filled that gap between visits and professional care is no longer needed.
Clinician Burnout Has Broken Through
Nurses and doctors are wasting a lot of time on documentation instead of care. This burden is alleviated by AI-assisted drafting, summarisation and workflow automation, which recaptures time, which is spent where it is most valuable, which is spending time with patients.
This overlap is the reason why ChatGPT-style health tools are leaving pilot projects behind and becoming everyday tools.
How Generative AI Is Changing Diagnostics Today
Diagnostics lie in the center of healthcare, and here the influence of AI can be felt. Generative AI is assistive to diagnostics in three major ways:
Pattern Recognition At Scale
AI models examine large volumes of data in order to uncover associations that humans can overlook. In imaging, this marks abnormalities. In laboratory data, it implies the identification of previous indicators. It is an act of relating dots over years of records in a patient’s history. AI does not diagnose alone. It helps clinicians to reduce oversight risk and focus narrowly.
Clinical Decision Support
Physicians are resorting more to AI-generated summaries that point to potential conditions, applicable guidelines, and new studies. This is not a substitute for expertise. It improves time-pressured situational awareness.
Early Risk Identification
AI is good at identifying minor trends. Minor deviation in vitals, behaviour or lab findings can be a sign of deterioration even before symptoms develop. Prevention is a life-saving expense.
The transition is not too dramatic, yet impactful: the diagnostics become proactive instead of reactive.
AI And Patient Care: From Appointments to Everyday Life
Patient care is no longer initiated and finished in the clinic. Generative AI to homes, phones, and workplaces: The care becomes more personalized.
- Smarter Symptom Guidance: Symptom checkers that are powered by AI now provide improved questions, respond to queries, and motivate next steps. They help reduce panic, sift misinformation and refer patients to prompt care.
- Individualised Health Education: Jargon confuses in the medical field. AI converts complicated terms into comprehensible messages depending on the understanding level. Patients are not overly informed.
- Chronic Conditions Support: In the case of individuals who need to manage chronic diseases, AI tools issue alerts, monitor trends, and reveal concerns in advance before reaching critical stages. This ongoing support helps in filling the lapses between appointments.
The outcome is not self-diagnosis. It is informed participation.
AI now extends patient care beyond the clinic, offering clearer guidance, simpler explanations, and continuous support; empowering informed participation, not self-diagnosis. (Image Source: MorphCast)
Within Hospitals: Where AI is Slipping Silently But Surely
One of the most complicated operating settings in society is the hospital. Generative AI currently performs behind the scenes, making it efficient.
- Clinical Documentation: AI writes notes, discharge notes and referrals, utilizing conversations and data inputs. Clinicians review and modify as opposed to creating new records.
- Triage and Resource Allocation: Triage systems, which are assisted by AI, help emergency departments to rank cases by risk, not by the order of arrival. This enhances performance in a stressful situation.
- Interdisciplinary Communication: AI summarises the patient cases in handovers to minimise information loss during change of shifts.
These transformations are not the subject of headlines, but they are changing the everyday provision of healthcare.
Reliability, Precision, and the Human Line AI Crossovers
Trust is central, even though fast adoption is evident. The healthcare industry requires more standards than the rest of the industries. Mistakes have actual ramifications.
It is due to this reason that the existing AI health systems focus on:
- Clear disclaimers.
- Advisory action to consult with the professional care.
- Evidence-aligned responses.
- Ongoing human oversight.
The field of medicine does not work autonomously with AI. It is decision support, but not decision authority. Clinicians do not lose their responsibility. Patients remain protected. Speed is not as important as this balance is.
Ethics and Regulation: Why AI in Healthcare is a Slow Mover
The healthcare innovation is not that of consumer tech, and it has a reason to be that way. Regulators focus on:
- Data privacy.
- Bias mitigation.
- Transparency.
- Accountability.
- Safety validation.
This regulatory climate makes the irresponsible use of deployment slow and reasonable development possible. It also determines the future of ChatGPT Health-style tools, as they should not undermine care. Healthcare AI does not triumph by going swiftly, but by going in the correct direction.

Healthcare AI moves carefully, guided by privacy, safety, and accountability; progress over speed. (Image Source: IIoT World)
The Bigger Picture: The Emergence in 2026
Generative AI does not come as a product or platform. It snips into the systems that people are already using. The actual disruption of ChatGPT Health and AI in medicine is not a disruption as such. It is restoration – restoring time, clarity, access, and balance in an overstretched system. Healthcare is still human in its essence. AI simply helps it breathe.
The Impact of Clinical AI Adoption: Pilot to Practice
There is a slow pace of experimentation with new technologies in healthcare. Such a warning is reasonable where human lives are at stake. But generative models, which were previously viewed as experimental, are now in standard clinical practice. AI is viewed with a warm but cynical reception in most hospitals. Here’s how adoption scales:
Embedded In Daily Workflows
Instead of being individual platforms, AI tools are becoming a part of the electronic medical records (EMRs), radiology suites, and telehealth platforms. Instead of accessing a separate application, clinicians can view AI summaries in addition to patient charts or imaging outcomes. This integration matters. It eliminates friction and will enhance trust since it does not seem like an external addition to the system but a part of it.
Specialised Clinical Modules
Now, health systems stop applying generic AI in all tasks. They implement specialised modules of:
-
- Cardiology.
- Oncology.
- Neurology.
- Emergency care.
- Diabetes management.
These modules incorporate clinical guidelines applicable to certain specialties, which further restricts safety and relevance. This is a focused method that enhances the performance and confidence of clinicians.
True-Life Success Cases: Life on the Other Side of the Hype
The worldwide initial applications demonstrate the ability to improve.
Case: Smarter Emergency Department Triage
One of the examples is a big city hospital, where AI is applied to prioritize emergency cases on the basis of their risk, but not the time of arrival. Rather than a long queue, patients who are in urgent need are served on the spot based on an AI risk score. Hospital staff report:
- Shorter wait times.
- Reduced the occurrence of important events.
- Better resource allocation.
Nurses view AI as a second pair of eyes that confirms their concerns and expedites care when needed.
Case: AI Support to Chronic Care Clinics
Within chronic clinics, such as diabetes and heart disease clinics, AI will assist patients in monitoring trends in glucose, blood pressure, drug levels and lifestyle diaries. When the trends undergo deviations that are not projected to improve, AI raises red flags that need attention by the clinicians before the symptoms are escalated. Patients define this empowerment as not intrusive but rather empowering.
The Collaboration, Not Replacement of the Healthcare Workforce in 2026
Among the most important questions is the question concerning people: Will AI replace jobs? The resolution to this is subtle and comforting, according to projections in 2026.
AI is Not a Replacement for Clinicians – It Redefines Work
Monotonous duties are replaced by AI:
- Drafting notes.
- Retrieving guidelines.
- Summarising records.
This leaves clinicians to work on human-only work:
- Emotional support.
- Complex decision-making.
- Patient counselling.
- Ethical judgments.
AI has become an ally of doctors, nurses, and allied health workers and administrators. In this cooperation, new positions are formed:
- AI health specialists.
- Optimisers of clinical workflow.
- Data-assurance coordinators.
- Digital health trainers.
The healthcare teams do not decrease their abilities.
Clinician Sentiment: Skepticism to Partnership
In 2026, surveys indicate that clinicians no longer feel threatened but relieved. There is a reduction in administrative load, documentation is not as tiring, and patient time improves. Physicians refer to AI as a safety net – the ability to screen minor errors before they escalate into major issues.
Building Patient Trust: The Nucleus of AI Adoption in Healthcare
In the context of healthcare, technology has to win trust more quickly and even deeper than in any other industry. In the case of the patients, trust will be established on transparency, accuracy, safety, respect for privacy, and clear boundaries. This frame takes AI in healthcare forward in 2026.
Transparency Comes First
The AI systems also give clear explanations now, like which data they used, what assumptions they made, and the reasons why they suggest some further actions. This is offsetting the black box fear that patients had towards the early AI systems.
Boundaries Remain Clear
Patients do not consider AI as a replacement for their clinician. Rather, they perceive AI as an assistant that offers insights, suggests next steps, and gives a background of education. Most importantly, patients will always see a tagline such as: “This fact will aid the assessment of your healthcare provider. Always seek the advice of your clinician to be diagnosed and treated.” These precautions enhance credibility and lower misunderstanding.

In healthcare, AI earns trust through transparency, clear guidance, and defined boundaries; acting as an assistant, not a replacement for clinicians. (Image Source: LinkedIn)
Ethics, Equity & Safety: A Responsible Way to Go
Healthcare is a sensitive and intimate land. The most critical issues of AI deployment are ethical ones.
Bias Mitigation
The patterns among underrepresented groups can be misunderstood by AI systems, which have been trained on uneven information. Responsible AI in healthcare in 2026 implies the constant audit, refinement, and remedy of bias. Various datasets that demonstrate age, gender, ethnicity, and regional health profiles are invested in health systems. This enhances efficiency and fairness.
Patient Agency
AI does not make patients make decisions. It informs choices. Patients are left with agency – with more focused and personal information. Before the integration of AI-generated insights into care plans, healthcare providers provide consent and make sure that the consent is made properly.
Security & Privacy
One of the most sensitive is health data. The standards of 2026 require encrypted storage, strict access controls, ongoing monitoring, and open data control procedures. The patients have the right to access their own data, know how it’s used, and request corrections or deletion of their data. This humanistic model will help this patient feel confident that AI will support care without invading dignity and privacy.
Global Adoption is not a one-size-fits-all
The use of AI in healthcare is growing at a global level, though the rates of its adoption differ.
Well-Resourced Systems
In developed health care systems, such as Australia, the USA, the UK, Singapore, and even some aspects of Europe, the advanced AI applications are incorporated into high-data, high-resource environments, with well-developed digital infrastructure. These systems lead to real-time diagnostics, clinical modules in specialisation, and automated workflow in hospitals. Australia is the country where both the public and private hospitals are actively implementing AI tools that help them to process triage, image interpretation, and documentation.
New And Underprivileged Environments
In less-developed areas, AI performs another task, which is to widen access. Here, AI supports remote consultations, basic diagnostic guidance, and local languages of health education. Nowadays, patients in numerous rural regions receive health assistance through AI-enhanced mobile services in the case of inadequate clinicians. The issue of infrastructure can still be a challenge, but AI fills gaps that previously appeared impossible.

AI in healthcare adapts globally: advanced systems enable real-time care in developed countries, while in underserved areas, it expands access and education. (Image Source: Brookings Institution)
Challenges Still Ahead
Despite development, there are still actual difficulties.
Overreliance Risks
There is a risk that doctors may start to use AI summaries without sufficient scrutiny. Mitigation involves strong oversight, frequent review of recommendations, and training on limitations. AI will be an assistant rather than a power.
Resource Disparities
Advanced AI does not fit into all systems. Equity in access is a universal concern. Subsidisation, optimisation, and scaling of affordable AI tools efforts are ongoing, though with mixed success.
Training & Literacy
Clinicians and patients should constantly learn what AI can and cannot do, how to interpret outputs, and how to spot errors. AI literacy has become part of healthcare training programs, in addition to other essential skills of a 2026 clinic that need to be included in healthcare institutions.
Practical Applications: Applications in the Real World
The concept of AI in healthcare is easier to understand through practice.
Example: A Patient Journey
Emma is 58 and has shortness of breath. The AI symptom support tool in her clinic poses specific questions and provides suggestions on the possible causes based on patterns, recent history, and summaries of guidelines. Emma makes an appointment for a telehealth meeting on the same day. Her clinician is provided with an overview of vital symptoms and risk flags generated by AI, which saves time and makes it more focused. The physician requests a specific examination and starts treatment promptly. Emma is listened to, ready and more enlightened. This isn’t science fiction. It’s everyday care in 2026.
Example: Clinician Support
Dr Khan begins her day with case notes that are summarized by AI and subsequently reviews them during morning rounds. She does not read long history books but reads a brief and precise summary of historical events compiled by AI. She is in contact with patients more and does less paperwork. Her job feels more rewarding.
The Future Horizons: The Next Frontiers of Healthcare AI
Although AI in healthcare is becoming part of the industry today, there is more change to come tomorrow.
Individualized Predictive Medicine
Instead of responding to symptoms, AI will more often anticipate health events in the future based on trends in genetics, lifestyles, and environment. This makes the possibilities available, including early risk reduction plans, individualized lifestyle prescriptions, and disease prevention-based models of care.
Real-Time Monitoring
The continuous monitoring of health is done through wearables, sensors, and mobile data streams that are fed into AI models, which do not work episodically but continuously. When deviations are made, alerts are issued. Clinicians act in the initial stages of intervention, decreasing hospitalization.
AI-Assisted Research
AI systems help in speeding up medical research through searching through literature in seconds, determining new correlations, and hypothesis proposals for clinical trials. This reduces the interval between discovery and practice.

Healthcare AI’s future: predicting health risks, monitoring in real time, and accelerating medical research for smarter, faster care. (Image Source: Forbes)
Practical Implications for Healthcare Professionals
As a health care system member, whether a clinician, an administrator, or a patient advocate, these are real steps which you may take in 2026:
- Embrace, Don’t Fear: Use AI as something that clarifies, makes things more productive, and insightful.
- Stay Critical: Apply AI outputs as formatted recommendations, which have to be checked by human beings.
- Educate Continuously: Invest in the development of literacy on technology, ethics, and interpretation.
- Prioritise Trust: Be transparent with the patients about the role AI plays in care and not replacing care.
Also Read: AI Makes Sleep a Disease-Prediction Tool of Modern Healthcare
Finally, an Anthropocentric Future
Generative AI in healthcare does not reduce the role of a human. It amplifies it.
AI facilitates comprehensible data. It reduces mundane tasks. It throws light upon complicated patterns. It enables the decision-making that clinicians and patients have to make at the end of the day.
The healthcare narrative in the year 2026 will not be about a human versus a machine. It is a machine with a human- it is oriented to the improvement of health outcomes, clarity of communication, and the system that is concerned about people, not paperwork.
Healthcare is a highly human activity. Technology just enhances humanity to be more effective.
Frequently Asked Questions (FAQs)
- Is ChatGPT Health replacing doctors?
Ans: It assists clinicians and patients but does not substitute professional diagnosis or treatment. - Are AI-driven systems as effective at diagnosing diseases?
Ans: AI supports analysis and pattern recognition but does not provide standalone medical diagnoses. - Is AI technology safe in healthcare?
Ans: When managed responsibly, AI enhances safety by reducing errors and supporting human supervision. - Is generative AI currently used in hospitals?
Ans: Many healthcare systems use AI for documentation, triage support, diagnostics, and workflow optimisation. - Will AI help reduce healthcare costs?
Ans: AI improves efficiency, which helps manage costs, but it does not replace the need for skilled human care.

