The Essential Facts First
Today, hospitals employ AI predictive tools to forecast the demand for the emergency department, sometimes weeks before. These systems examine live data, as well as historical data, including patient arrival patterns, weather, seasonal illnesses, public events, staff numbers, and bed availability.
The result is quite simple but effective. They know when the pressure points will come and how strongly they will hit. This ability enables them to better allocate staff, open beds earlier, re-route ambulances, and improve waiting times in A&E. In the year 2025, the way emergency care is delivered changes from reaction to anticipation.

AI tools now help hospitals anticipate patient surges, easing pressure on A&E departments in 2025 (Image Source: Mandelbulb Technologies)
Despite Progress, A&E Waiting Times Are a Major Priority
As the NHS continues to evolve, emergency departments remain at the cutting edge of the healthcare field. However, every delay carries consequences. Longer wait times pose clinical risks, affect the morale of healthcare workers, and cause distress for patients and relatives. These wait times create system-wide delays altogether.
Demand is rarely uniform. Epidemics occur during winter and reach sudden peaks. Weather conditions can cause cardiorespiratory arrest, holidays alter patterns of injury, and even sports tourism can overwhelm a local emergency room. Conventional planning approaches have difficulty keeping up; spreadsheets and historical means simply will not react quickly enough. AI can.
What is Different in AI Forecasting Than Traditional Planning?
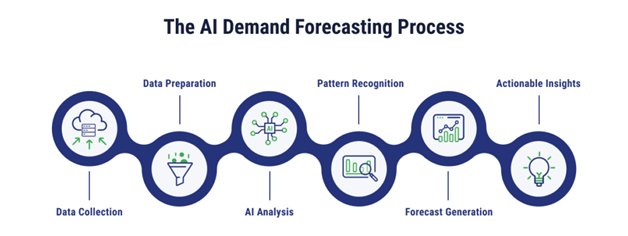
Forecasting in the healthcare system is not something new. What has changed in 2025 is the accuracy, quickness, and scalability. AI models process huge amounts of data and learn patterns that the human eye cannot detect quickly.
These systems learn endlessly, making adjustments to the predictions as new data is received. Contrary to static forecasts, AI models change every hour. Their adaptability makes them the best for emergency care environments, where situations change very quickly.
How AI Forecasting Tools Actually Work
Fundamentally, these models are based on machine learning algorithms trained on many years of hospital data. They analyze a wide variety of inputs:
- Hourly emergency department volume
- Acuities of patients
- Ambulance dispatch data
- Weather forecasts
- Seasonal illness trends
- Public events and holidays
- Staffing rosters
- Bed occupancy rates
The model finds correlations. For instance, a low temperature combined with increased cases of the flu means that there will be a large number of respiratory admissions soon. Artificial intelligence does not displace clinical judgment; it strengthens it.
AI models analyse hospital data to predict emergency surges before they happen (Image Source: TierPoint)
Real-Time Forecasting: A Paradigm Shift
By the year 2025, hospital administrators will not wait for moments of crisis to take action. AI dashboards provide hourly and departmental projections of patients. This understanding enables leadership teams to:
- Increase the number of employees before peak periods
- Postpone elective surgeries temporarily
- Open overflow units pre-emptively
- Optimize triage workflows
- Make arrangements with ambulances
This leads to a smoother workflow for patients, with fewer queues. Patients notice the difference right away.
The Human Impact Inside Emergency Departments
There are people behind the technology. Now, doctors no longer go into their shifts “blind.” They plan for forecasted peaks instead of functioning solely in crisis response. Paramedics also avoid long offload delays.
These modifications lead to a reduction in burnout. They offer a means of controlling an environment that has hitherto been controlled by unpredictability. Artificial intelligence forecasting doesn’t eliminate pressure; it redistributes it intelligently.
Why 2025 is a Turning Point
Several elements are at play this year that have made AI forecasting a standard:
- Data Maturity: The healthcare industry currently has enough clean and digitized data to train effective models.
- Infrastructure: Cloud infrastructure now supports the heavy lifting of real-time processing.
- Staff Trust: The trust of the staff in AI tools increases as the accuracy of the predictions is proven in daily practice.
- Funding: Governments and healthcare networks are embracing predictive analytics funding.
What was experimental before now seems necessary. AI forecasting is now fully integrated into conventional emergency response activities.
AI Forecasting vs Generative AI In Healthcare
Public interest is often drawn to chatbots and medical language models, but forecasting uses different models. These systems operate behind the scenes. They are hardly noticed because they have no fancy interfaces or public conversations.
However, their effects do not end there. These factors influence staff structure and allocation and directly affect patient outcomes. This explains why health systems are focusing more on forecasting and not necessarily just on conversational AI.
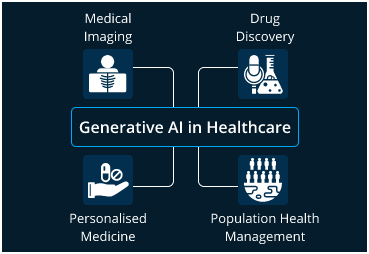
Unlike chatbots, AI forecasting works quietly in the background, shaping staffing decisions and patient outcomes. (Image Source: LeewayHertz)
Data Quality is the Spinal Column
The best predictions made by AI are only as good as the data feeding them. In 2025, healthcare facilities spend significantly on enhancing data flow to ensure these systems function at peak performance. This involves formalizing coding conventions, integrating previously siloed systems, and meticulously cleaning historical datasets.
Quality data leads to better forecasts and, crucially, higher clinician confidence. Trust in technology increases exponentially when forecasted results consistently correspond to real-world experience.
How AI Forecasting Directly Reduces Waiting Times
Waiting times decrease through several specific operational shifts:
- Aligned Staffing: Coverage corresponds to actual anticipated demand rather than static historical averages.
- Bottleneck Identification: Patient flow is enhanced because potential clogs in the system are identified hours before they manifest.
- Ambulance Offload Efficiency: Delays in ambulance handovers are reduced when the hospital expects arrival surges and clears space in advance.
- Effective Bed Management: Bed management teams can plan discharges more effectively, ensuring a constant “pull” through the system.
These factors accumulate, turning saved minutes into hours of avoided delays for the average patient.
Reducing Waiting Times Enhances Outcomes
Shortening waiting times has an impact that transcends improving patient satisfaction levels; it directly reduces clinical risk.
- Early Assessment: Faster access to clinicians prevents patient deterioration.
- Faster Triage: Rapid processing leads to fewer adverse events while waiting.
- Infection Control: Shorter queues mean less crowding, which directly reduces the risk of cross-infection.
AI-based forecasting indirectly benefits patient safety by optimizing the environment in which care is delivered, without actually intervening in the clinical treatment itself.
Mitigating Concerns Regarding AI in Emergency Situations
Skepticism remains a healthy part of medical progress. Many professionals are wary of algorithm dependence and data privacy. To address these concerns in 2025, hospitals have incorporated radical transparency into their tech stacks:
- Explainable AI: Systems describe how models function and which factors influenced a specific prediction.
- Human-in-the-Loop: AI serves as a decision-enabler rather than a decision-driver, keeping clinicians in control.
- Regular Audits: Hospitals perform frequent audits of prediction accuracy to prevent bias or “drift.”
AI Does Not Replace Experience
Experienced practitioners recognize nuances that AI might miss. Veteran staff understand local culture and shifts in the “feel” of a department that data may not yet capture. These human skills are enhanced, not replaced, by forecasting tools. The best possible results are achieved when human judgment and machine insight operate in tandem.
The Global Relevance of AI Forecasting
Every emergency hospital faces similar structural challenges regardless of location. Urban hospitals struggle with overcrowding, while regional centers deal with staff scarcity. Low-resource environments often face the most unpredictable surges. Because AI forecasting adapts to local data, it enables more intelligent resource allocation irrespective of the hospital’s size or location. This universality is currently fueling instantaneous adoption worldwide.
Forecasting Meets Real-Time Decision Systems in A&E
The true utility of AI exists where predictions interact directly with existing hospital technology. Current technologies enable the integration of forecasting models with live dashboards in emergency operation centers. These dashboards can:
- Update patient volume projections in real time.
- Adjust forecasts dynamically as new data arrives.
- Provide push notifications to clinical leads hours or even days before peak times.
This allows managers to rearrange allocations mid-shift. For example, if a forecast predicts high admission rates six hours in advance, a lead clinician can call in additional staff and expedite administrative discharges before the queue even begins to form.
The Role Of Environmental and External Data
At the core of these models exists a variety of diverse data sources. Weather conditions, community health data, and even traffic patterns are now used to predict emergency demand. For instance, the combination of a heat wave and an increase in influenza cases allows models to predict high volumes of respiratory emergencies. This gives hospitals the window needed to prepare beds and ambulance services well before the crisis hits.
Governance and Ethics: Predicting Without Compromising Trust
As forecasting techniques become standard, issues of governance are paramount. Hospital administrators must ensure systems remain confidential and undergo constant audits to avoid inaccuracies. These measures include clear indications of data sources and robust protections for data privacy.
Notably, prediction software does not displace clinical judgment. The software supports operational decisions while the healthcare team maintains overall responsibility for patient carea balance essential for maintaining trust in high-stakes emergency settings.

Strong governance ensures AI forecasting supports care without compromising trust or clinical judgement. (Image Source: LinkedIn)
Reducing Administrative Burden and Supporting Staff
Other than predicting demands, most AI solutions simplify administrative work. Predictive models can also automate shift assignments, provide recommendations regarding bed assignments through flow predictions, and even predict length of stay based on patient information. This allows medical professionals to focus on practicing medicine rather than navigating administrative hurdles.
Hospitals using these systems have noticed marked improvements in wait times and patient satisfaction by incorporating predictions directly into hospital triage and bed flow processes.2 Because emergency department units are high-stress environments, anything that facilitates administration acts as a positive factor for staff well-being.
Case Study: Royal Melbourne Hospital’s Predictive Modelling
Predictive modelling activities are on the rise in Australia. The Royal Melbourne Hospital, together with the University of Melbourne, is pioneering research-based initiatives that help model the estimated length of stay for patients within the ER.
These models also predict patient disposition, whether a patient will be sent home or admitted to a ward. Even in its research phase, this work illustrates how predictive systems interface with electronic records to forecast care patterns and eliminate delays. From queue forecasting to patient pathway predictions, the role of emergency operations is increasingly becoming one of rapid reaction and adaptability.

Australian hospitals are testing predictive models to forecast emergency stays and patient pathways. (Image Source: The Royal Melbourne Hospital)
Global Adoption Beyond the NHS
While the UK National Health Service is a leader in implementing these predictive tools, the movement is a global phenomenon. Hospitals in the USA and Europe use such models to forecast patient flow and admissions. Evidence verifies that prediction systems focusing on short-term horizons, such as six hours, clearly improve the ability of ERs to prepare for demand.
In the Asia Pacific region, technology partners are testing solutions that consider local outbreaks, climates, and unique healthcare habits. This flexibility allows forecasting solutions to adapt to the specific service models adopted by different health systems.
Forecasting and the Wider Health System
Emergency departments are not stand-alone facilities. Forecasting impacts hospital discharge, referral, and admission processes, which are the primary drivers of ED demand feedback loops. For instance, when a hospital forecasts a potential influx, it can increase the rate of ward discharges to create capacity.
This approach reduces the cycle time from the point of emergency entry until final treatment or release. It also carries significant implications for ambulance provision; knowing when congestion is forecast allows workload management to prevent delays when time is most crucial.
What Research Shows
Scientific research and academic work confirm the observations made by practitioners. Recent models developed in university collaborations, such as deep learning models for forecasting emergency room boarding volumes, have demonstrated that AI can lead to substantial improvements in planning. These models provide information beyond what can be achieved through traditional manual planning by analyzing operational metrics like queue length, bed usage, and arrival frequency.
Display Challenges and Constraints
Forecasting methods are potent, but they are not flawless. Their efficacy relies on:
- The quality and completeness of the underlying data.
- Ongoing maintenance and recalibration of algorithms.
- Successful incorporation of models into the clinical process.
Hospitals with fragmented digital data may find it challenging to install these systems. Furthermore, transparency remains an issue; forecasts must be understandable to the clinical team to ensure trust. Organizations are now prioritizing “explainable” models where the reasoning behind a forecast is clear to the user.
The Economics of Forecasting in Emergency Care
Reductions in waiting times and streamlined operations have significant cost consequences. By predicting pressures accurately, hospitals can avoid last-minute changes and the high expenses associated with agency nurses.
Efficient bed management leads to fewer unnecessary admissions and shorter lengths of stay, reducing overall costs. Furthermore, forecasting decreases the indirect costs associated with clinical deterioration and the cancellation of elective surgeries due to overcrowding. These savings often form a beneficial cycle, allowing for reinvestment into care quality.
Also Read: AI-Powered Smart Homes Failing in 2025: Risks of Generative AI
Future Outlook: Forecasting as a Standard
Forecasting methods may become a common feature in emergency response by the end of 2026. Major events on the horizon include:
- Predictive triage systems that forecast both the volume and urgency of incoming patients.
- Integration with wearable devices and community health data to forecast surges before they reach the hospital.
- Cross-system networks aid regional health systems with resource allocation.
- Visual dashboards that empower clinical leaders with forecast-driven decision support.
Final Thoughts
Forecasting methods in emergency care signify the transition from chaotic response to strategic planning. They assist in managing hospital demand, decreasing waiting hours, and improving staff support. In 2025, these are no longer fringe science projects but fully functional systems with measurable effects. As data quality and model development continue to improve, the applications for reshaping emergency healthcare will only expand.
Frequently Asked Questions (FAQs)
- What is AI forecasting in emergency healthcare?
Ans: AI forecasting employs machine learning to predict patient demand and resource pressure in emergency departments by analysing real-time and historical data. - How accurate are AI forecasts for hospitals?
Ans: Accuracy increases when models are trained on real-time data. Many current models are capable of predicting surges with very small margins of error. - Does AI substitute doctors and nurses within A&E?
Ans: No. AI assists in planning and operational functions, while all professional and clinical decisions remain human-driven. - Can AI forecasting minimize ambulance delays?
Ans: Yes. By predicting surges in arrivals, hospitals can prepare resources and bed space before ambulances actually arrive at the scene. - Is patient data secure in AI-based forecasting systems?
Ans: Yes. Hospitals adopt strict governance, data anonymisation, and advanced security measures to ensure the privacy of patient information. - Can forecasting tools project demand beyond 24 hours?
Ans: Yes. Some models can predict several days into the future, although precision is typically highest for shorter-term prediction periods. - Are forecasting systems effective for smaller hospitals?
Ans: The tools can be scaled to regional contexts, though an integrated data infrastructure is a necessary prerequisite for effectiveness. - What is next in forecasting after emergency departments?
Ans: Hospitals are investigating opportunities in patient admission planning, surgical services scheduling, and discharge coordination. - Are these tools expensive to implement?
Ans: Costs vary, but the improvements in waiting times, staff productivity, and patient outcomes often justify the initial investment.

